8-minute read!
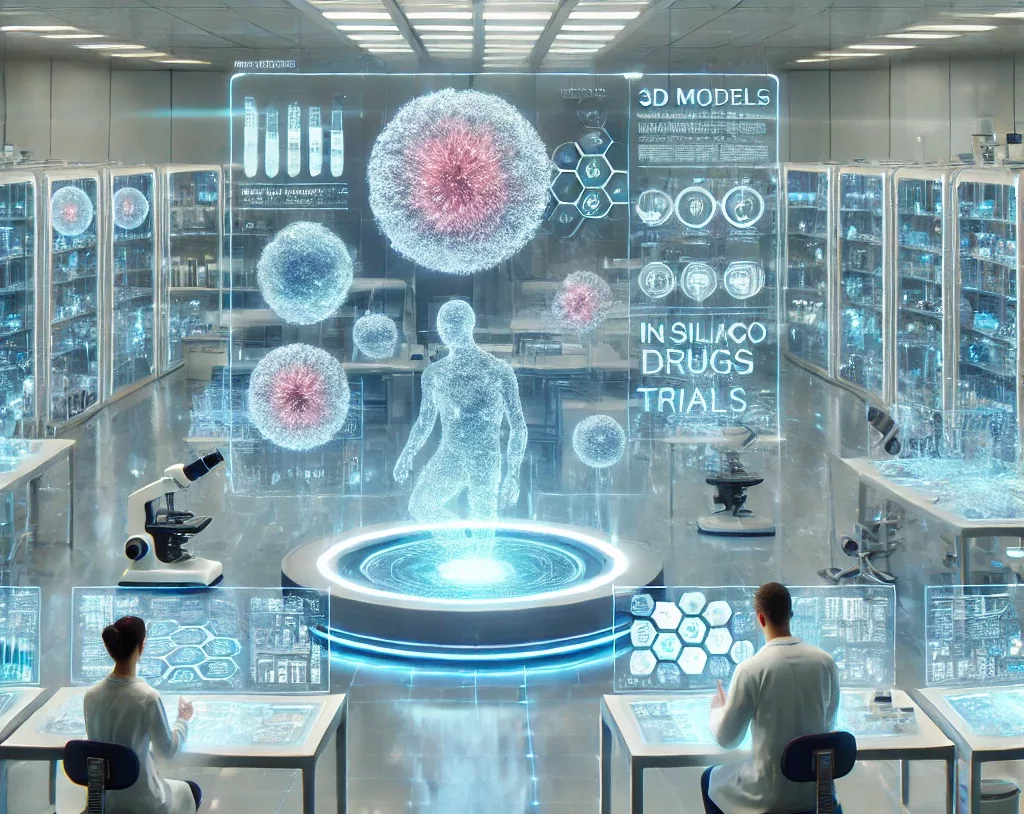
The digital revolution has transformed every aspect of our lives, including biomedical research. A major leap forward is the rise of in silico trials—computer simulations that replicate how drugs or medical devices interact with the human body.
Imagine a lab without test tubes or microscopes, replaced by complex algorithms and virtual models of human physiology. This isn’t science fiction; it’s the new reality reshaping medical research. Yet, as these digital breakthroughs redefine healthcare, they also introduce a critical challenge: navigating the evolving regulatory landscape, particularly in the European Union, where striking the right balance between innovation and robust legal frameworks is essential to unlocking the full potential of in silico trials.